40yr male
This E-log also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan.came to the hospital with
CHEIF COMPLAINTS: of breathlessness since 20 days
Cough since 20 days .
HOPI: patient was apparently asymptomatic 20 days back later he developed breathlessness MMRC grade 3 not associated with wheeze , no orthopnea, PND aggravated more on sleeping on left side, relived wen Lying down on right side
Cough non productive , associated with chest tightness , loss of weight, loss appetite since 20 days
Low grade fever with evening rise of temperature, associated with chills and rigors, relieved on medication
No complaints of chest pain , palpitations ,decreased urine out put , was admitted in pulmonology department on 2/11/22 and being followed up by general medicine department in view of elevated trop I 310, ecg changes showing deep T inversions in V1- V6 leads, P- pulmonale QT- 0.4 secs.l
On 4/11/22
7:20 pm the case was transferred to general medicine in view of 2Decho changes RWMA+,LAD akinetic LCX&RCA hypokinetic, EF - 40 , for further evaluation and management
Past history:
History of similar complaints 20 days back , treated locally
K/c/o Pulmonary TB.( Sputum positive in 2020 )used, ATT for 2 months later stopped
And started again since 20 days
K/c/o RVD positive detected 2020 , used for 2 monthsTlD+ Doltogravir and stopped later, and started 20 days back.
Not a known case of DM,/HTN/CAD/epilepsy
Personal history:
Pt is lorry driver by occupation
Diet: mixed
Appetite: decreased since 20 days
Bowel and bladder movements: regular
Sleep : adequate
Addictions: consumes regular alcohol 180ml per day since 20 yrs
Chews guttkha 1 packet per day since 20 yrs
General examination:
Patient conscious, coherent, cooperative
Well oriented to time place and person
No pallor.Noicterus,cynosis, clubbing,lymphadenopathy ,odema
Vitals:
Temp : 99.7f
Bp:80/60mmhg
Pr:104bpm
Rr:40 cpm
Spo2 - 74 @ ra
96with 4 liters of o2
Grbs:166
SYSTEMIC examination:
CVS: S1,S2 +
Respiratory system:
UPPER RESPIRATORY TRACT:
NOSE: no dns; polyps
Oral cavity: poor oral hygiene
Posterior pharyengeal wall:normal
Lower respiratory tract:
Shape of chest -bilateral asymetrical,
Right side chest muscle mass- loss of suppraclavicular and infraclavicular hallowness
Left side chest movements decreased
No crowding of ribs,
Wasting of muscles-ve Usage of accessory muscles+
Spinoscapular distance equal on both sides.
palpation: all inspectory findings confirmed,No local rise of temperature
Apex beat felt at inch medial to MCL
Tactile vocal fremitus equal on bs
Percussion:
Direct percussion: resonant on clavicle and manubrium
Indirect percussion:resonant in all areas and dull on left lower lobe
Auscultation:Auscultation
BAE+(decreased breath sounds on left lower lobe)
B/l Crepts present on supraclavicular infraclavicular,midaxillary,infra axillary,supra scapular,infra scapular
PROVIOSIONAL DIAGNOSIS:
RIGHT UPPER LOBE, LEFT UPPER LOBE LOWER LOBE CONSOLIDATION LEFT UPPER LOBE CAVITY 2° to TB? PCP WITH RVD+
investigations :2/11/22

TREATMENT
INJ THAMINE 1 AMP IN 100 ML NS/IV/BDA
ATT 3 DRUGS PER DAY UNDER NTEA
ART TLD+ DOLTOGRAVIR
INJ PIPTAZ 4.5 GM IV/TID
INJ HYDROCORTISONE 100 MG IV
INJ NORAD @ 8ML PER HR
INJ CLEXANE 40 MG SC BD
INJ LASIX 40 MG IV/BDIF SBP >= 110MMHG
TAB ECOSPIRIN 75MG PO/OD
TAB BACTRUM DS OD/PO
TAB PCM 650 MG PO BD
SYRUP GRILLINCTUS OX 2TSP PO TID
CAD (triple vessel disease) HFrEF with (EF EF-48%) WITH LEFT SUPERIOR PULMONARY VEIN THROMBUS WITH TYPE 2 RESPIRATORY FAILURE SECONDARY TO B/L PULMONARY .T.B. ON ATT WITH ?SUPER INFECTION WITH ? PCP WITH ? CAP VTH RVD +VE ON ART
































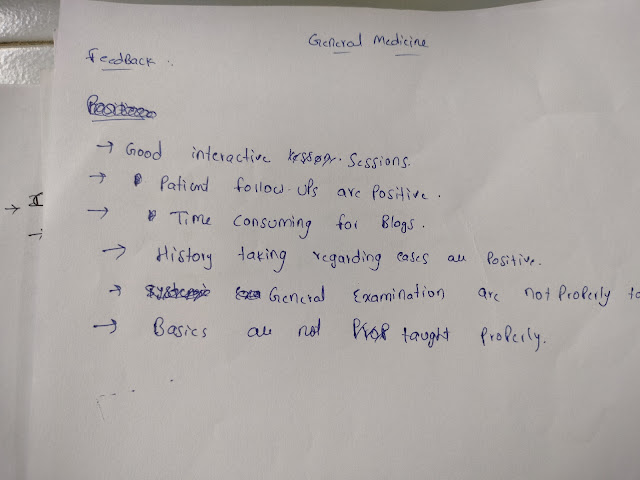

Comments
Post a Comment